
Four years ago, Dr. Victoria Claydon, who specializes in cardiovascular function after SCI, set out to answer some basic questions about bowel care and its impact on autonomic dysreflexia (AD) and people’s quality of life. Claydon, who is an ICORD researcher and an associate professor at Simon Fraser University, knew that bowel management is a common trigger for AD for people with injuries above T5. But she wanted to get a better handle on the extent of the problems and, in the process, understand how people’s bowel management affects their quality of life.
A better understanding, she reasoned, could make it easier to target aspects of bowel care that could be modified to lessen the risk of AD—and improve quality of life. With her colleagues, she developed a survey to consult the best experts in the field—individuals living with SCI. Given the very personal nature of bowel care, it’s probably not the easiest subject for people to answer questions about. Nevertheless, over the course of three years, 287 individuals committed to taking part in the survey. Of these, 210 answered every question.
The majority of respondents—55 percent—were Canadian. Their ages ranged from 20 to 84, with time since injury ranging from eight months to 49 years. Approximately 67 percent of respondents had an injury at or above T7 (making them at risk for AD), and the majority of injuries (63 percent) were incomplete.
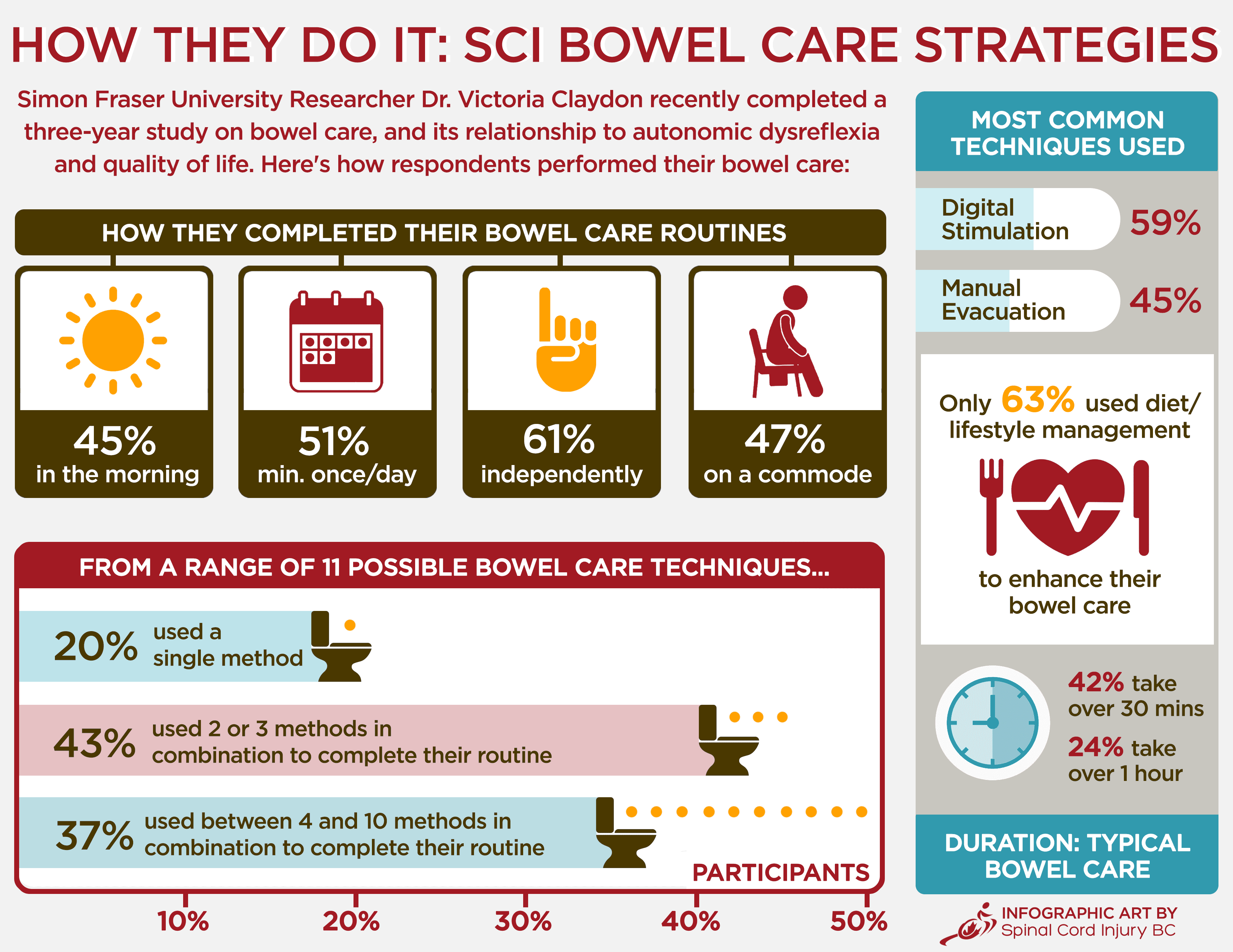
Any way you look at them, the results paint a stark picture of just how big of an issue bowel care is for people with SCI. Bowel management was a problem for 78 percent. It interfered with personal relationships for 60 percent of respondents; 62 percent said it prevented them from staying away from home. The normal bowel care duration was greater than one hour for 24 percent of respondents. About 33 percent reported experiencing bowel incontinence at least once a month. Of those with injuries above T7 and at risk for AD, 74 percent had AD symptoms during bowel care. AD interfered with activities of daily living in 51 percent.

“We learned a lot from this project,” says Claydon. “I think we had the sense before we started this survey that bowel care represented a source of frustration for individuals living with SCI. However, I think the level of concern and the extent of the need for improvement in bowel management has been underestimated. The negative impact of bowel care on quality of life was profound. Bowel care was reported to have a worse effect on quality of life than bladder care, sexual dysfunction, pain, spasticity, using a wheelchair for mobility, and skin integrity concerns.”
Another result that resonated with Claydon was the confirmation of just how often bowel management is a trigger for potentially deadly episodes of AD (see side- bar for the physiology behind this connection). “About two thirds of those surveyed had high-level injuries that put them at risk of experiencing AD, and of these, 79 percent reported symptoms of AD that were triggered by their bowel care, including 32 percent who experienced palpitations,” she explains. “Those who experienced AD during bowel care commented that episodes of AD interfered with their social activities, activities of daily living, work, exercise and sleep.”
Perhaps one of the most eye-opening findings for Claydon was that, despite a high level of dissatisfaction with bowel care, and frequent and troublesome episodes of AD, 71 percent of respondents had not made any changes to their bowel care for at least five years.
“This,” says Claydon, “highlights gaps in bowel management education, and raises questions about current guidelines for bowel management. Ongoing support and education is essential for continued effective bowel care management, especially as changes in gastrointestinal and cardiovascular function occur over time after injury and with aging, demanding ongoing adaptations to routine management protocols. Our study demonstrates the need for better information and resources about this topic for individuals with SCI and their caregivers, and better consideration of where individuals with SCI and their caregivers obtain information about this topic.”
There are other important findings of the study that Claydon points out. The negative impact of bowel care on quality of life was greater in those who took a long time to complete their program, or who had more severe AD. Bowel care was also associated with poorer quality of life in those with higher level injuries, those with more complicated (more techniques) bowel care routines, and those with more severe fatigue.
“We also found that 71 percent of individuals intentionally restricted their fluid intake to help with their bladder management, despite the risk of worsening blood pressure control through poor hydration, and worsening bowel care by exacerbating constipation,” she adds.
But Claydon says there is good news: now that she and her colleagues have a better grasp on these issues, they can suggest some ways to improve bowel care immediately, and can also move forward with research intended to find ways of improving bowel care and associated quality of life.
“As a first step, we would encourage individuals living with SCI to discuss their bowel care and any associated cardiovascular concerns with their caregivers, to see if there are measures they can take to improve it,” she says. Among the possibilities are finding ways to optimize bladder care that rely less on limiting fluid restriction, and implementing strategies to reduce both the time taken to complete bowel care and the number of approaches needed to complete bowel care.
“We also have two new projects that will help address these concerns,” continues Claydon. “The first is a study that is looking at whether we can better manage episodes of AD that are triggered during bowel care, and whether this will improve quality of life.”

This study involves a trial to determine whether using a lubricant gel that contains local anaesthetic can block some of the sensory stimulus triggered by bowel care and, in the process, prevent or reduce AD episodes. Participants wear a blood pressure monitor while they conduct their usual bowel care, with privacy, in their own home on two different days. On one day they will use the medicated lubricant, and on the other day they will use a regular lubricant without anaesthetic. (Note that this study is currently seeking participants; see page 33 for more details.)
“We also just received funding from ICORD and the Rick Hansen Foundation to further examine the barriers that lim- it individuals with SCI making changes to their bowel care,” says Claydon. “In this project, we will conduct interviews with individuals with SCI, their families, and caregivers to examine the barriers that limit making changes to their bowel care. This will increase our understanding of barriers to change, establish a rationale for further more in-depth research, and generate a framework for change for affected individuals, caregivers and health organizations that will guide improvements in bowel management.” SCI BC is pleased to be a partner in this research project.
In the world of SCI research, studies examining the secondary complications of SCI often take a back seat (with apologies) to projects that focus more on a “cure” for SCI. But as this study by Claydon confirms, the priorities of people living with SCI are often at a disconnect with SCI cure research. We commend her and her colleagues for tackling issues like this.
We were curious about Claydon’s personal motivation to conduct a study like this—particularly given the length of time required to complete it.
“That’s what research is all about,” says Claydon. “Recognizing that it can be a long and tumultuous journey, but trusting that the idea is important, and that ultimately the results will help transform understanding and improve people’s lives. I think there are often two main reasons why researchers pick a particular area to study. One is that the area is intellectually stimulating—there is a puzzle or a problem that intrigues and piques their attention. The other is that there is a sense that the answer will have meaning, either to an individual, society, or a body of scientific understanding. We embarked on this project for both reasons.”
As this issue of The Spin was going to press, Claydon’s research was about to be published in the Journal of Neurotrauma with the title of “A community perspective on bowel management and quality of life after spinal cord injury: the influence of autonomic dysreflexia”. Visit the Journal of Neurotrauma for more details.

This article was originally published in the Winter 2017 issue of The Spin. Read more stories from this issue, including:
- Martial Arts
- Exercise Guidelines
- 60th Anniversary
And more!
Read the full Winter 2017 Issue of The Spin online!



