Whether you call it pot, weed, marijuana, or grass, cannabis is sparking interest like never before. In fact, research suggests that one in three people with SCI in Canada are already using it—and 60% of those use cannabis daily. But is cannabis a cure-all or just another passing puff?
Since legalization in 2018, the landscape has shifted dramatically: more research, more products, and more Canadians using cannabis. Here at The Spin, we want to help you navigate the world of cannabis, whether you are a cannabis newbie or a regular toker.
We’ll start by breaking down the latest research, introduce you to common cannabis terms, and share stories from peers about how cannabis fits into their lives.
CANNABIS CONFUSION
Step into a cannabis store these days and it can feel overwhelming. Miyah Kailey says, “As someone who uses cannabis chronically, even I think, what is happening? What does this mean? I couldn’t even imagine wanting to use for the first time or having a specific goal in mind. It’s hard to figure out what you want when cannabis comes in so many different forms now.”
Kailey, a student in Dr. Kathleen Martin-Ginis’ SCI Action Canada lab, completed her Bachelor of Health and Exercise Science (Honours) at UBC Okanagan in April 2025. Before moving onto her next adventure studying Occupational Therapy at the University of Alberta, she spent the summer compiling the best available research on cannabis and SCI.

She started by talking with peers at SCI BC and Accessible Okanagan events in Kelowna. Kailey explains, “When I shared that I was also a chronic user, a lot more people would come out about their experiences. I really wanted to make a space that was non-judgmental, very inclusive, and would facilitate that conversation around cannabis while making sure that I’m not giving incorrect information.”
Kailey notes while research on cannabis and SCI exists, it’s still in its early days. Many studies involve only small groups of participants. Dosing recommendations are not yet well supported by evidence. Kailey focused on gathering evidence-based information.
THE ENDOCANNABINOID SYSTEM: HOW DOES CANNABIS EVEN WORK?
Let’s break it down.
Think of your neurons (nerve cells) as chatterboxes, constantly passing notes back and forth. They use chemicals called neurotransmitters to send these messages across tiny gaps, called synapses, from one neuron to the next. For the message to land, the neurotransmitter (the key) has to fit perfectly into the receptor (the lock). This is called neurotransmission. Depending on the receptor, the neuron can either get excited (speed up) or inhibited (slow down).
We all have an endocannabinoid system, which helps us recover from stress and maintains balance across our body systems. When we experience stress, this system kicks in and sends ‘messages’ (cell signaling) that help our body relax, eat, sleep, forget the stressor, and protect from stress.
Cannabinoids are chemical substances that connect to the cannabinoid receptors in the body and brain. Our bodies naturally produce endocannabinoids (endo meaning inside). Some examples of endocannabinoids are Anandamide (AEA) and 2-Arachidonoylglycerol (2AG). Cannabinoids can also come from outside the body, such as the Tetrahydrocannabinol (THC) and Cannabidiol (CBD) found in cannabis.
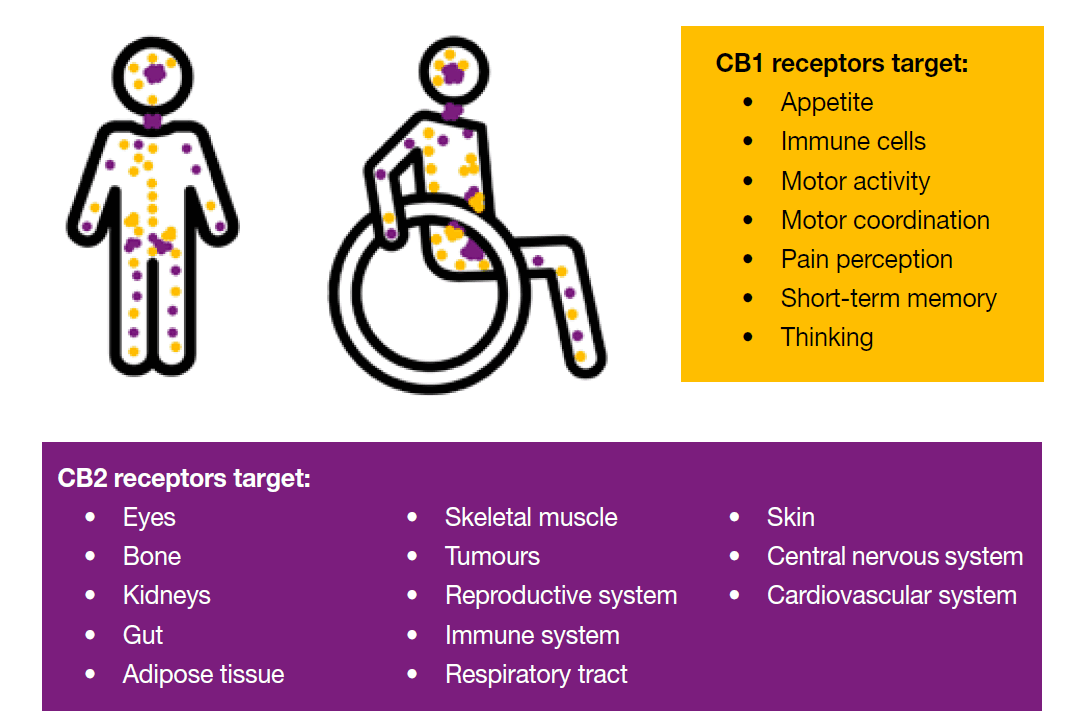
The endocannabinoid system is made up of more than just endocannabinoids and the enzymes that clear them away when they’ve done their job. It also includes two main types of receptors: CB1 and CB2. These receptors are associated with specific bodily functions.
When our endocannabinoids system kicks in, AEA and 2AG (endocannabinoids) bind to the CB1 receptor, telling the presynaptic neuron to slow the release of neurotransmitters. Once the endocannabinoids signal the cell to slow down, they are eaten up by enzymes (MAGL and FAAH) and regular neurotransmission resumes.
What causes the endocannabinoid system to kick in? Well, anytime the body experiences stress, this system kicks in to help us recover and return to baseline.
When we add cannabis to this system, things get complicated. CBD is a non-psychoactive cannabinoid and has therapeutic benefits (more on these benefits later). In contrast, THC is a psychoactive cannabinoid that gives us a ‘high’.
When THC enters the system, it connects to the CB1 receptor (the same receptor AEA and 2AG bind to) telling the presynaptic neuron to slow the release of neurotransmitters. This time, there is no enzyme to eat up THC. Because the THC lingers in the system, this leads to lasting neurological effects which is referred to as the ‘high’.
When CBD is introduced to the endocannabinoid system, it changes the shape of the CB1 receptor when it binds. Now when THC goes to bind to CB1, it does not fit as well into CB1 because of the shape change. Using CBD + THC has been thought of as a method that reduces the ‘high’ when compared to using THC alone.
That was a lot of information, so let’s summarize it in a few points:
- Neurons talk to each other using neurotransmitters.
- When our body experiences stress, our endocannabinoid system kicks in and tells the neurons to slow down how much they talk to each other (less neurotransmitter release).
- When THC enters the system, it also tells the neurons to slow down their talking but, there is no enzyme to eat up THC, so we get lasting neurological effects (‘high’).
- When CBD enters the system, it changes the shape of the CB1 receptor. This doesn’t let THC fit as well so it cannot tell the neuron to slow down as much as it wants to. It is thought that this reduces the ‘high’ from THC.
Check out the video and diagram below for further explanation.
The Endocannabinoid System: Further Explained
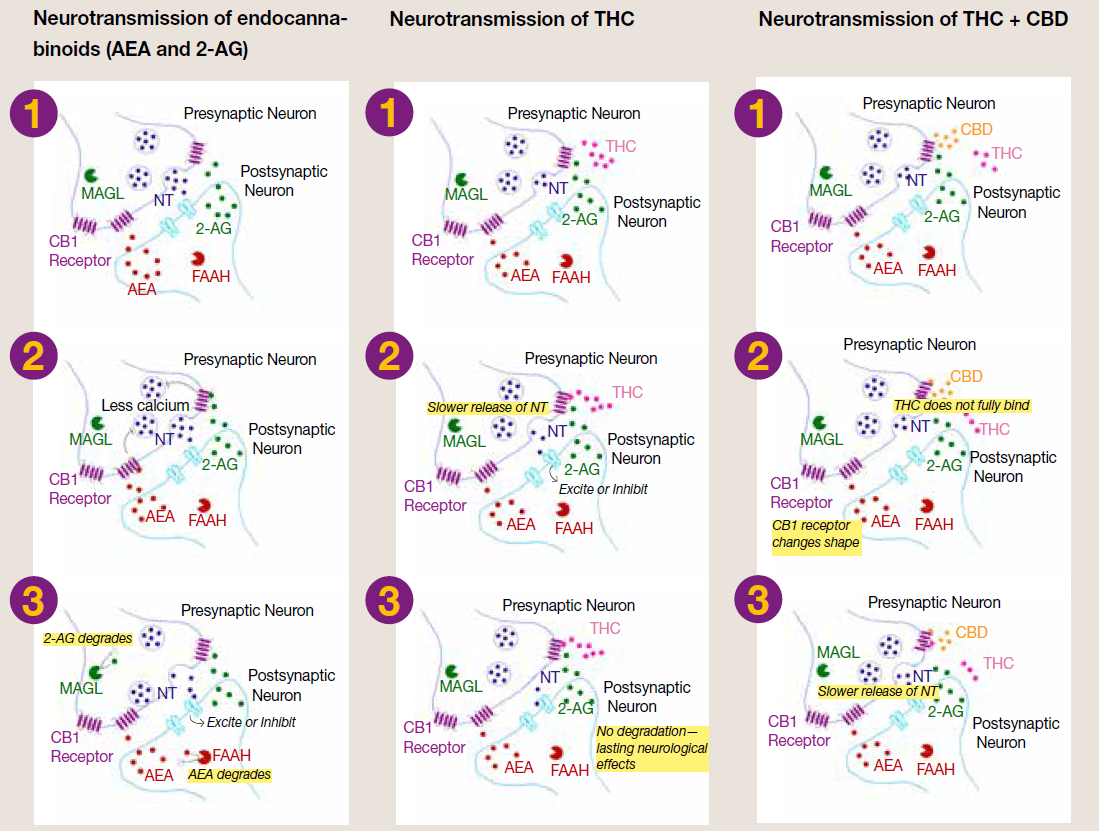
Normally, when a neuron is activated, high amounts of calcium trigger the release of neurotransmitters (NTs; like serotonin or dopamine). The presynaptic (first) neuron releases the NTs which then bind to a receptor on the postsynaptic (second) neuron. The NTs tell the postsynaptic neuron to speed up or slow down and neurotransmission continues.
Neurotransmission of endocannabinoids: When we’re stressed, the body makes its own cannabinoids (AEA and 2AG). They bind to CB1 receptors on the presynaptic neuron, telling it to release less calcium and therefore fewer NTs. This helps calm things down. The enzymes FAAH and MAGL then break down AEA and 2AG.
Neurotransmission of THC: THC also attaches to CB1 receptors on the presynaptic neuron, telling it to release less calcium and slow down NT release. But unlike AEA and 2AG, THC isn’t quickly broken down by enzymes, so the effects last longer and creates a ‘high’.
Neurotransmission of THC + CBD: THC and CBD both bind to the CB1 receptors on the presynaptic neuron. CBD changes the shape of the CB1 receptor, so THC can’t attach as strongly as it normally would. This means THC can only send a weaker signal to ‘slow down’ NT release. The presynaptic neuron still reduces calcium release, but only partially. As a result, the overall effect of THC is blunted, and the ‘high’ is less intense.
DIFFERENT CANNABINOIDS AND THEIR BENEFITS
You might be familiar with the terms indica and sativa:
- Indica: A strain of cannabis that is thought to be relaxing or aid in sleep, typically for nighttime use.
- Sativa: A strain of cannabis that is thought to be uplifting or euphoric, typically for daytime use.
- Hybrid: A strain of cannabis that is a cross of sativa and indica, the effects may vary depending on the amount of sativa and indica.
Today, most cannabis has been crossbred (mixing of two plants) so it’s unlikely that a strain is purely an indica or sativa.
When choosing a cannabis product, it is important to know what effects each cannabinoid may have. Remember that everyone’s body is different. A cannabinoid that helps someone else may not produce the same benefits for you.
THC is the cannabinoid most people associate with cannabis. It’s psychoactive (meaning it changes how you think or feel) and is responsible for the ‘high.’ THC can produce calm, reduce perceptions of pain, increase appetite (the ‘munchies’), and reduce spasticity in some individuals.
CBD doesn’t cause a high. Instead, it may reduce anxiety, ease inflammation, relax muscles, promote sleep, and is also used medically to treat epilepsy.
CBN (think N for night) has sedative properties and may help with both falling and staying asleep. It can also reduce anxiety, promote relaxation, reduce the perception of muscle pain, stimulate appetite, and preliminary research suggests it may help with glaucoma.
CBG tends to be more uplifting and may temporarily improve depressive symptoms. It may reduce inflammation, improve gut health, and preliminary evidence in rats suggest that it could have neuroprotective effects (i.e., protect neurons from injury or degeneration).
You may come across other cannabinoids like THCV, THCA, and CBC; however, there is not enough research yet to describe their potential therapeutic benefits, especially for people with SCI.
LET’S TALK ABOUT TERPENES
Terpenes are another term that come up in the cannabis conversation.
These natural compounds give cannabis (and other plants) their aroma and flavour. Lavender, for example, gets its relaxing scent from the terpene Linalool which is linked to easing anxiety and inflammation.
Cannabis contains more than 150 different terpenes! Some of the most common include Myrcene, Caryophyllene, Limonene, and Terpinolene. You’ll often hear claims that specific terpenes help with pain, sleep, or mood, but most of this evidence is either anecdotal or from early animal studies.
There’s also the entourage effect: the idea that cannabinoids and terpenes work better together than alone. Products labelled “full-spectrum” contain multiple cannabinoids and terpenes, while “isolates” contain just one.
Kailey’s advice? “If you’re a chronic user, I would pay attention to the terpenes. If you’re not, I wouldn’t say that’s the most important part.”
A practical tip: If you try a product and like it, write down how it made you feel. Later, look it up online (leafly.ca has a helpful strain database) to see its cannabinoid and terpene profile. You may notice you prefer certain cannabinoids and terpenes, and this can help you pick out products that work best for you.
THE REASON PEOPLE WITH SCI USE CANNABIS
So why are people with SCI turning to cannabis? Many who use it describe reasons ranging from recreation to managing anxiety, stress, depression, bladder and bowel issues, nausea, appetite loss, sleep problems, and relaxation (sources: 1, 2, 3, 4, 5, 6)
A survey of 156 people living with SCI in the United States who routinely use cannabis found that the most common reasons for cannabis use were managing pain and reducing spasticity. In Canada, a survey of 80 people with SCI revealed similar trends. The top reasons were reducing pain (36.3%) and improving sleep (30%), followed by reducing spasticity (20%), reducing the need for other medications (16.3%), reducing stress/anxiety (15%), reducing depression (13.8%), and recreation/enjoyment (10%). The main reasons cited for not using cannabis were concerns about negative health effects and social stigma or fear of judgment.
It’s important to note, however, that many individuals with SCI report no improvements with cannabis use. In the Canadian study, participants rated the effectiveness of cannabis for pain relief an average of 53 out of 100, and 68 for sleep. Promising, but far from conclusive.
At this point, there are no large-scale research studies that definitively test whether cannabis is effective for these purposes in people with SCI.
THE MANY WAYS TO CONSUME CANNABIS
Cannabis isn’t one-size-fits-all. Whether you puff, pass, vape, bake, or drop a little oil under your tongue, there are plenty of ways to consume. Among Canadian peers who use cannabis, edibles are reported as the most common method, followed by smoking and vaping.
Common inhalation methods include joints, vape pens, pipes, and bongs. If hand dexterity is a challenge, you can buy pre-rolled joints (‘pre-rolls’) or cones to fill with ground cannabis. Spliffs and blunts are similar to joints but also contain tobacco. Vape pens are usually rechargeable and vaporize oil in a cartridge (‘cart’) or you can pack flower into a dry herb vape.
Edibles come in all shapes and sizes: gummies, chocolate, beverages, baked goods, tinctures, and more. In Canada, the total THC content in an edible package can’t exceed 10 mg, which is plenty for some and barely enough for others. Edibles take longer to kick in, but some companies make “fast-acting” versions by pre-metabolizing the cannabis, so your body absorbs it more quickly.

There are different risks and benefits associated with both ingesting and inhaling, so let’s break some of them down:
INHALED | |
Benefits | Risks |
|
|
INGESTED | |
Benefits | Risks |
|
|
NEGATIVE SIDE EFFECTS OF CANNABIS
Like any substance, cannabis comes with risks. Side effects can include paranoia, feeling less ‘in control’ of your body, nausea, dry mouth, drowsiness or dizziness, altered taste, increased anxiety, lack of motivation, and potential interactions with medications.
Long-term use may lead to tolerance, dependence, and symptoms
of withdrawal when discontinued. And for anyone with impaired autonomic, cardiovascular, or respiratory function, regular monitoring for any changes is crucial.
CONCLUSIONS ON CANNABIS
Research on cannabis and SCI is still new. The studies that exist are small and based on self-report, which does not prove that cannabis is effective for pain or spasticity. High-quality research with large numbers of participants is still needed.
So, will cannabis work for you? The best answer we can provide with the current research available is that we don’t know, it might and it might not.
Read on to hear from peers about their experiences with cannabis.
RUSS’ STORY: SLEEPING SOUNDLY
Russ Dolton never thought he’d use cannabis. Growing up as a national level rower, stories of clogged lungs kept him away. “I don’t like to have anything control me other than my obsessive work ethic,” he says.
10 years ago, a cycling accident in Port Coquitlam left him with an SCI. His late wife was a huge support, and together they made sure the injury didn’t affect their relationship.
Like many readers of The Spin, Dolton struggles with neuropathic pain and spasms that wrecked his sleep. “I was sleeping and waking up after three or four hours. I couldn’t get a consistent night’s sleep,” he says. He tried everything from meds to meditation.
When cannabis was legalized in 2018, he figured, “I’ve got nothing to lose, so why not?” When he broached the topic of cannabis, his “strict, old school” doctor said no and prescribed more pills. Since then, a younger, more open physiatrist reassured him, ‘I’m not a pot advocate but do whatever works for you.’”
Some friends were initially skeptical and, “thought that I was going to the dark side, which was kind of comical,” Dolton says, but overall, “I find that people are accepting.” For those who don’t agree, he adds, “That’s your problem, not mine. I really don’t care what you think, this is what helps me. You don’t have my issues, so you don’t understand.”
Dolton is mindful of his use, especially with “addictive personalities” in his family. While Gabapentin and Baclofen help during the day, it’s nighttime when pain hits and cannabis provides relief. “When I’m being distracted [during the day], I really don’t notice. At night when I’m winding down, that’s when I notice the twitching and the jumping impact my life,” he explains. “Having that vape at night helped to give me at least six to eight hours of sleep, which was a blessing because I was waking up tired all the time. I’ve got sleep apnea as well as a result of my SCI. The vape helped me pass me through that section of waking up all the time and give me a consistent night’s sleep.”
It took some trial and error to find what works. Edibles didn’t suit him. “The delay on those was just incredible! I took one, then another. Well, this is not even working. So I took three! The next day I woke up and I didn’t hear my alarm. I was in la la land and kind of dopey,” Dolton says. “I can’t control the residual effects of the gummies. I prefer something that acts quickly so I can moderate it, rather than waiting for the aftereffects.”
Rolling joints was a “ridiculous endeavor” for Dolton. “Bouncing and falling on the floor. It was making me more irritated trying to do it,” he laughs. Now he uses leftover flower in a pipe but mostly relies on a vape pen. He doesn’t like smoke clogging his lungs, and a couple of puffs from the pen each night is all he needs to get a restful sleep.
Dolton also acknowledges the realities of living with a disability on a limited income. When he does smoke, he does so on the porch of his BC Housing rental. “I don’t smoke a lot, so there’s not a lot of residual pot smell,” he says. When it comes to buying cannabis, Dolton says the cost is worth it for the relief it provides. He explains, “I can’t afford to go spending a lot of money. I’ve got certain amount of disposable income like $300, $400 a month that I can play with. It’s been somewhat of a barrier, but it’s not a lot. I spend $50 to get a cart for my THC pen. I just bought one three weeks ago. I’ve still got it and it looks like there’s a lot in it. It’s probably going to last me a month, maybe two. I can live with that.”
Dolton is happy to share his experience with fellow peers struggling with pain or insomnia. He shares, “One guy said he was always afraid to try it because you don’t know where you’re getting advice from. I mentioned I don’t hit it hard and it’s just from a therapeutic point of view… I have introduced a couple of my friends, and they said it’s the best thing that ever happened to them.”
Today, Dolton is sleeping well and active in the disability community. He regularly attends SCI BC events and is part of the advocacy group Equal Access Collective.
CHRISTOPHER’ STORY: CANNA-BUSINESS
Christopher Bryan knows cannabis—it’s literally his business. “I had my medical grow license for 16 years and now I have opened The Green Den, a retail cannabis store in Scotch Creek,” he explains.
A freehand climbing accident as a young adult left Bryan with an incomplete L3/L4 injury. He shares, “I have kind of exceptional levels of pain because of how low my level of injury is. It’s been a really long journey for me to try and find stuff to help relieve pain. I’ve seen 18 different pain specialists over the last 21 years. I use both traditional means of pain management with cannabis as a little extra.”
Getting there wasn’t easy. When Bryan first applied for a medical grow license in the early 2000s, a fill-in doctor accused him of being a “drug seeker.” The irony? “The doctor prescribed me a whole bunch of oxy. So, you’ll give me medical heroin, but you won’t give me medical cannabis?” His regular doctor later approved the license, and with help from friends, Bryan started growing.
His parents, both in the medical field, were supportive. “They’re very open to the actual medical benefits [of cannabis]. They don’t really have that old school mentality,” says Bryan. He’s even helped his dad find products for shoulder pain.
Bryan stopped growing about eight years ago, once more products became available on the grey market (i.e., retail stores open before legalization). “It wasn’t worth the extra effort of growing,” he says. These days, he prefers tincture oils and creams and rarely smokes. “I used to be a lot more recreational [with cannabis], but I stopped smoking and drinking and just trying to live healthier and cleaner. Putting anything in your lungs is not good for your lungs. That was my only concern with long-term use.”
Medications such as Gabapentin and Lyrica came with unwanted side effects, Bryan recalls. “I’ve been able to eliminate a lot of traditional medication for different types of cannabis products.”
CBD and CBG work best for Bryan’s pain. He adjusts his dose depending on his pain level. “If I’m having a bad day of pain, I’ll take like 100 mg of CBD, probably three or four times throughout the day. And I’ll also take usually about 50 mg of CBG in the same intervals. That usually helps with the inflammation that’s causing my pain. And I’ll put cream on my back a couple times a day if my pain is really bad.”
At The Green Den, Bryan’s lived experience with pain makes him a trusted guide. Shoppers come in looking for relief, and they listen when he shares what’s worked for him. “I’ve been consistently getting people for sleep and just directing them the right direction that they need to go has been rewarding in itself,” he says. He also ensures his team is just as knowledgeable, keeping them trained on cannabinoids, terpenes, and new research.
Still, Bryan says the cannabis industry has room to grow. “It’ll take another five or ten years before the industry is really where we all want to see it at.” Testing standards, in particular, need attention. “Right now [companies] can get all their weed tested from like 15 different facilities with different results from each one. They shop around for whatever testing facility is going to give them the best numbers. They need to be more regulated,” referring to the cannabinoid concentrations listed on packaging.
But overall, he’s seen big improvements since legalization. He explains, “At first, they were just hiring anyone that could grow plants, but they didn’t hire people that knew how to grow cannabis. It took them a while to realize that to get quality products, they need people that know how to grow cannabis. A lot of them started hiring legacy growers and have their own research teams.”
“The quality of products has gone up so much even in the five years that my store has been open. When we first opened, I had to be very careful on what I was ordering because some of the companies were so inconsistent with quality. Now, the quality is more consistent,” Bryan says. Some companies are even developing mildew-resistant strains.
So, what advice does Bryan have for peers curious about cannabis? “Think about what you actually want to get out of the product before you start using it, because it’s a whole different product based on what your needs are.” He stresses the importance of getting information from multiple sources and making sure it matches up.
Bryan adds, “Start slow. Don’t try to get super high the first time. Start with lower THC stuff or even like the THC + CBD combinations, because it’s a more relaxing experience and easier to ease into… Now CBC and THCV are starting to become more popular, which is really good to see because I find those to be the most beneficial for neurological disorders. I’m glad to see
more products coming out with those minor cannabinoids.”
MICHELLE’S STORY: FINDING STILLNESS
“In general, I play pretty fast and loose with cannabis,” says Michelle Kam. She lives with quadriplegia caused by multiple sclerosis (MS); she now uses a power chair full-time. For Kam, the line between therapeutic and recreational use of cannabis is blurry. “That’s how dealing with the MS has gone. I’ve had days where I didn’t get to smoke weed and I lived, but that is not how I would like to live. I prefer to start my day with a smoke, because then you’re good and high and everything else goes nicely.”
Kam started smoking cannabis with a partner, but when the relationship ended, she faced a new challenge. She explains, “I didn’t know that many people that smoked weed. Because of being quadriplegic, I need help smoking weed. I started lining up people to smoke with.”

Like some peers, Kam is much younger than most residents at her long-term care home. Earlier this year, she transferred to a new residence in Kelowna, and the change has been a game-changer. “I had come from place where cannabis was so against the rules. They thought everything I brought into my room was an edible. I was policed for everything. Now I’m at a place where it’s no problem,” she says. At her previous home she relied heavily on others. Now, she has her distillate pen within reach, “from the moment I’m up in my chair to the moment I go to bed.”
With that change, her anxiety and her cannabis use has gone down. “I actually smoke way less now… When I lived at the last place and I couldn’t have it all the time, on the drive home I was hitting the distillate like crazy because I knew that it was going away until tomorrow or the next time I had a friend coming.” Still, she’s mindful of her intake: “I’m always worried about things like tolerance because you don’t want to keep chasing that dragon.”
Two years ago, after her breakup, Kam says her consumption was heavier. “I was smoking and drinking a lot. I told my doctor I don’t see myself quitting pot and alcohol. I can do one… I don’t believe in lying to your doctor or your lawyer.” Her doctor’s advice was blunt: “Pot all the way. You can’t OD on smoking pot.” Cannabis can cause an unpleasant “green out” but won’t stop you from breathing. By contrast, alcohol and opioids in high amounts can depress respiration and cause overdose. The choice was clear, Kam says, “I didn’t want to drink that much anymore. I didn’t want to be putting those calories into my body.”
And the therapeutic benefits of cannabis keep her coming back. “When I smoke a joint the spasms stop. It is so nice to just have about an hour of blissful stillness. When you’re constantly moving, you’re looking for stillness pretty badly,” she explains. Cannabis also helps her body relax for ceiling lift transfers. “The way that my body spasms and shakes and does its thing is not conducive to a great position in the chair,” she says. “I do use [cannabis] recreationally, but if it were up to me, that would be what I would use for my pain control for the MS.”
She rarely notices side effects, other than dry mouth which she manages with water and mouthwash. Smoking and quadriplegia bring some risk, she explains, “At the beginning of the joint I have no problems holding it straight and not burning myself. However, halfway through I stop paying as close attention to where my fingers are and one time I did burn my myself badly,” She adds with a laugh, “My dexterity is getting better, and I credit a lot of that to pot.”
Kam rotates between different forms of cannabis, though smoking is her favourite. She shares, “I am very blessed in that my mom grows for me, my mom rolls for me, and my mom grinds the powder for me.” Together, they pick indica strains that ease her spasms and pain. She starts most mornings with an edible powder mixed into pudding. “I used to do yogurt, but yogurt has to be refrigerated, and pudding does not,” she explains. She keeps her distillate pen handy on a lanyard around her neck throughout the day.
And when she treats herself at a dispensary, Kam can’t resist messing with the budtenders, “I often tell the kid behind the counter I want to go back to full quad when I smoke the joint.”
These stories show there’s no one path with cannabis. It may all seem hazy at first, but with curiosity and care, cannabis can become a useful part of your toolkit.
Read more stories from the Fall 2025 issue of The Spin, including:
- Virtual tours
- Entrepreneurship
- Catheter coverage advocacy
And more!





