What if we told you that a daily sprinkling of a fine white powder on your open pressure ulcer might cut the healing time in half, or even more? If you think we’ve lost the plot, we wouldn’t blame you. In fact, we’d be happy if this was your reaction, since we believe in science here at SCI BC—and the basis for all good science is healthy skepticism.
But we’re keeping an open mind about Amicapsil, a compound developed in the UK that’s based on something called MPPT, short for micropore particle technology. You may want to do the same. Amicapsil has a growing number of highly satisfied end users with SCI, mainly in the UK. Yes, it’s true that anecdotes do not constitute conclusive proof. But there’s also a growing amount of scientific evidence to support Amicapsil—enough to suggest that there may be something to it, and that, given the enormous implications of pressure ulcers, it needs to be investigated fully.
STAGGERING COSTS, NO TREATMENTS
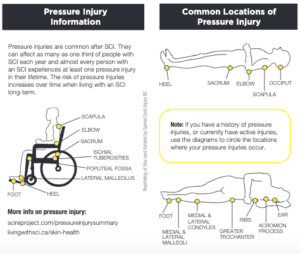
People with SCI aren’t the only ones prone to pressure ulcers, but we think it’s probable that no one is impacted more by them. Lack of muscle mass below injury means people with SCI lack “padding” to prevent pressure ulcers. Lack of sensation means those with SCI often don’t know they’ve injured themselves or that a pressure ulcer is getting more serious. And it’s recognized that people with SCI have compromised immune systems that makes it easier for pressure ulcers to become serious. Learn how SCI changes your skin, and how to protect and care for your skin post-injury, and download your wallet card that can can be given to your medical team to ensure proper care is taken.
The costs of pressure ulcers are enormous—to individuals, and to society. On an individual level, a serious pressure ulcer can stop us in our tracks, with the only remedy being weeks, months or even years of bedrest. On a societal level, costs are estimated to be a whopping $490 million per year.
Despite this, it might surprise you to learn that there’s no gold standard for treating pressure ulcers—particularly deeper wounds that refuse to close and heal. Nor has there ever been any game-changing research or treatment breakthroughs.
What we’ve known for some time is that, once infected, pressure ulcers become difficult to close and heal. Not surprisingly, health professionals have looked to antibiotics and antiseptics to stem infections, and still do. But several recent summaries of existing research have raised serious doubts about these approaches. One, published in 2016 by the highly skeptical Cochrane Library, concluded that, “There was no consistent evidence of a benefit to using any particular antimicrobial treatment for pressure ulcers.”
BACTERIA: FRIEND OR FOE?
Recently, there’s been some research findings that are changing our understanding of how pressure ulcers and other wounds heal. At the heart of this is a growing realization of the importance of our skin’s microbiome—an ecosystem of bacteria, fungi, viruses, and mites. When balanced, it’s an integral part of our body’s defence against infections.
In a serious pressure ulcer, the skin’s microbiome can be compromised, allowing one or a few bacterial species to take over. This constitutes an infection, which slows or even stops healing. Our immune system tries to prevent this, but rampant bacteria secrete toxins and enzymes to thwart immune cells and attack other beneficial types of bacteria. And the infectious bacteria also secrete a biofilm that creates a slime wall “fortress” around themselves that our body’s immune cells can’t penetrate to do their job.
Simply put, attempting to “carpet bomb” the infection with a topical broad-spectrum antibiotic or antiseptic might kill the culprit bacteria—but also all the other tiny living things essential for healing that make up our skin microbiome. In the case of antiseptics, even new cells at the wound site can be killed. There’s also growing concern about drug-resistant bacteria. Today, most of us carry at least one resistant strain of bacteria on our skin. The risk is that, with antimicrobial treatment, the resistant type will not be harmed, but the non-resistant types will be killed. So antimicrobial treatment can actually provide the resistant bacteria with ideal conditions to aggressively multiply and infect the wound.
REBALANCING THE MICROBIOME
All of this suggests that a better approach to healing difficult pressure ulcers would be supporting the immune system as it attempts to regain some balance in the microbiome at the wound site. This is exactly what MPPT does according to the company that developed it, the UK’s Willingsford Healthcare. Co-founded by Dr. Frank Sams-Dodd and his wife Jeanette, who holds a dual degree in business administration and veterinary science.
Sams-Dodd, a neuroscientist with 25 years of experience in the pharmaceutical and medical device industry, explains that Amicapsil is composed of “fine, highly porous particles that absorb wound exudate into a micropore structure.” He says that the micropores act as pumps, which are powered by evaporation—the exudate, or pus, which contains the toxins and enzymes secreted by infectious bacteria as weapons against the immune system, is drawn from inside the wound to the surface, where it evaporates. The removal of these toxins and enzymes allows the immune system to recover and regain control to balance the microbiome—necessary for healing.
Additionally, “Amicapsil does not contain any antimicrobials and is nonpolluting. It consists exclusively of natural non-toxic ingredients. It is readily biodegradable and can go directly back into the biological cycle.”
HOW TO USE AMICAPSIL
Treatment consists of first rinsing the wound with tap water, in the shower or with a squeeze bottle. Once dry, Amicapsil is applied directly to the wound. Only clean procedures are required. The wound can be left uncovered, or covered with a piece of gauze, providing it’s breathable to allow airflow and evaporation. The frequency of treatment depends on the severity of the pressure ulcer and the healing progress.
In 2016, Amicapsil was approved for use by professionals in the UK and throughout the European Union. In 2017, approval was extended for use by individuals. It has similar approvals in Australia and New Zealand. There are no formal approvals in Canada or the US, but there’s nothing to stop people in North America from importing it for personal use.

WHAT THE SCIENCE SAYS ABOUT AMICAPSIL
There’s way too much research to attempt to summarize in detail here but we’ll provide a few highlights. In a 266-patient randomized clinical trial in the UK, Amicapsil was compared to the antibiotic gentamicin and the common antiseptic iodine in abscesses, surgical wounds, venous leg ulcers and diabetic foot ulcers. The study showed that it removed wound infections 60 percent faster than both the antibiotic and the antiseptic, and reduced the number of hospitalization days by 31 percent.
Moreover, in a UK case-series study of 40 acute or chronic wounds and pressure ulcers in people with SCI. According to Sams-Dodd, Amicapsil closed all the pressure ulcers, regardless of whether they contained resistant bacteria or not, as long as the person started treatment before the wound was two months old. The older the pressure ulcer was, and the more antimicrobial and antiseptic approaches that had already been tried, the longer healing took. In many wounds over six months old, the infection had spread to the bone, but even with these, Amicapsil was able to remove the infection in the soft tissue.
A deep dive into the most recent case study, led by Dr. Oliver O’Sullivan at the Defence Medical Rehabilitation Centre (DMRC), the UK’s national rehab facility for injured military personnel reveals more success. O’Sullivan’s case study subject, a service man in his 30s, had sustained a complete SCI in 2016. In early 2019, he developed an abscess. Despite several aggressive interventions including surgery, the abscess turned into a serious non-healing wound over the course of seven months. That, of course, took an enormous toll on the physical and mental health of the patient, who eagerly agreed to the Amicapsil treatment. There was a dramatic improvement in the wound after one month—it no longer produced a foul odour, and it had reduced in size significantly. “We were surprised by the progress, especially at first,” says O’Sullivan. “It was clearly making a difference. After a month, we, and the patient, really felt it was worth pursuing as it was clearly improving this chronic wound and enabling him to undergo more rehab and improve holistically.”
AMICAPSIL IN THE REAL WORLD
Amicapsil has been approved to purchase since 2017, so it’s not surprising that many people with SCI have tried it and reported success.
One real life example, is 38-year-old Raquel Siganporia, a personal injury lawyer based in London who sustained a T6/7 injury 27 years ago. She first used Amicapsil two years ago for a small, open breakdown in the IT area (the two bones that are the lowest point of the pelvis when you’re sitting). Amicapsil helped this heal in 24 hours. “However, the biggest test was a skin breakdown following a misjudged transfer where the skin on the back of my thigh broke,” says Siganporia. In total, it took six weeks for Amicapsil to fully heal the pressure ulcer, which was about five cm long and 2.5 cm wide. “I have no doubt that using Amicapsil sped up my recovery and substantially reduced the amount of time I had to spend on bedrest compared to how long it has taken for other skin breakdowns in the past,” she says. “Amicapsil is life-changing, and I now keep a bottle in my fridge for whenever I might need it.”

THE CHALLENGES AHEAD FOR AMICAPSIL AND PRESSURE ULCER TREATMENT
Will Amicapsil revolutionize the treatment of pressure ulcers? We think it’s too early to say. But if it’s to do so, we believe there are three major hurdles that need to be addressed: no insurance coverage combined with what could be perceived as high cost, lack of awareness, and perhaps most importantly, the need for more research and conclusive evidence.
Let’s start with cost. At first glance, it is expensive—about $100 for a 750 mg bottle. Sams-Dodd says that smaller wounds can be healed with one to three bottles, with more complex wounds needing more. For many, this might simply be too much. But conversely, for anyone who has ever experienced a non-healing wound and the weeks and months required to heal, the cost might not seem that high. Completing more conclusive research will be necessary for health policy-makers to get on board.
Dr. Oliver O’Sullivan, the principal investigator of the most recent SCI case study of Amicapsil, agrees. “I think further studies need to be done before it will be widely adopted, and we are at the early part of this new developments journey.” One possible issue is that most of the research on Amicapsil to date has been funded and overseen by the company that makes it, Willingsford Healthcare.
We’re not suggesting the research is flawed or compromised, but we do think more independent research may remove any suggestion of conflict of interest.
For his part, Sams-Dodd is aware of the need for more research—but he points out that RCTs (randomized clinical trials) are difficult to design for products like Amicapsil. “We have discussed an RCT (randomized clinical trial) with the major SCI centre in the UK, but the choice of comparator has turned out to be the main challenge for everyone because it raises serious ethical questions,” he says, “The justification for an RCT is highly questionable in the absence of an effective gold standard, and even more so when it is predictable that the patients are highly likely to deteriorate if they use the common or standard approach.”
Sams-Dodd also thinks it would be difficult to find RCT participants. “In one treatment group, you have a product that has shown to have 100 percent efficacy in acute wounds, and in the comparator group you have something that has been shown to be ineffective and that everyone in the community knows this. Who would consent to participating?”
HOW TO GET YOUR HANDS ON AMICAPSIL
No doubt, some of you have been reading this and thinking, “OK…I need to try some of this!” The good news is that you can purchase Amicapsil directly from the company and also receive consultation on treatment.
However, we know it’s likely that, if you’re suffering from a serious pressure ulcer, you’re working with your own medical team towards resolution, and you’ll want to ensure any treatments are supported and approved by them. The problem is that it’s highly unlikely that more than a few health professionals here in BC have heard of Amicapsil, let alone any experience with it. So, you might have to take the lead in terms of encouraging members of your health team to learn more about it.
If you move forward with this, Willingsford Healthcare is willing to review daily photos and offer guidance to you, or to your family member or carer who is handling the treatment, via e-mail.
“This has developed into a more formalized telemedicine approach, which we currently are pursuing because it allows anyone to use Amicapsil independently of where they are in the world,” says Sams-Dodd. “Everyone who has used the approach has been extremely positive because it allowed them to control when and where to do the treatment.”
Amicapsil can be purchased directly from Willingsford Healthcare. For more information, visit willingsford.com or email contact@willingsford.com.
A final request to readers: if you decide to try Amicapsil, please let us know about your experiences with it so that we, in turn, can let other peers know by emailing jmaffin@sci-bc.ca.

This article originally appeared in the Winter 2020 issue of The Spin. Read more stories from this issue, including:
- The Comeback Cowboy
- Research on Exercise and Pain Management
- Winter Activities from our Community Partners
And more!
Read the full Winter 2020 Issue of The Spin online!