“I’ve had trouble managing my weight for a while now. It’s starting to affect my transfers and exercise is difficult with my shoulder injury. I hear about Ozempic everywhere lately, is it an option for someone with SCI? The side effects I’ve heard about make me nervous.” —Nic in New Westminster
We asked Dr. Ian Rigby, MD FRCPC, Diplomate of the American Board of Obesity Medicine, Emergency Medicine doctor and SCI Peer.
I’m not surprised you’re asking about Ozempic in this situation, Nic, as this and other weight loss medications have revolutionized how we approach the treatment of unhealthy weight. A few years ago, my wife and I were sitting in the airport waiting for a flight when I noticed a 12-foot digital billboard with the caption, “Ask your doctor if Ozempic is right for you.” As an obesity medicine doctor, I thought, “Here comes the rush…”
The medicine we’re talking about here is semaglutide, a once-a-week injectable medicine that comes in two forms. Ozempic is the form Health Canada approved for the treatment of diabetes, and Wegovy is the one for weight loss. They are the same drug, and which one is used clinically is unimportant.
“Is Ozempic right for you?” can be a challenging question. With all medications, we want to use them in situations where the benefits outweigh the risks and side effects. When using semaglutide for weight loss, we say that the medication is “indicated” for people with a body mass index (BMI) greater than 30 or for people with a BMI greater than 27 and with other medical conditions that would improve with weight loss (such as diabetes, high blood pressure, etc).
This definition can be challenging for those of us with an SCI. First, BMI is a crude tool that requires only height and weight measurements to screen for unhealthy weight. In the SCI population, BMI is often not an accurate measurement. Many of us have decreased muscle and bone mass, and as such, the BMI calculation often causes us to miss people who actually have an unhealthy weight. Furthermore, measuring height and weight in SCI can be impractical. Thus, your doctor may use other approaches to decide whether semaglutide may be an appropriate treatment.
Does it work? Yes. Depending on what study you read, the average weight loss for a patient using a top dose of semaglutide will be between 15 and 20% of their body weight. Granted, none of us are the average of a study. Some will lose more and some will lose less. Regardless, this is a profoundly effective therapy.
Perhaps the most important way semaglutide works is by causing the hunger and appetite circuits of our brain to make us less hungry. Second, it signals our stomach and small intestine to slow down, and we feel full earlier when eating. Finally, semaglutide also improves the body’s glucose metabolism which is used to treat diabetes, but may cause small weight loss benefits.
So, if semaglutide is so great, why isn’t everyone on it? First, there are some medical conditions that don’t go well with this medication. Your doctor would review your history regarding certain types of thyroid cancer, endocrine issues, and types of pancreatitis that would exclude you from using it. Second, these medications really require a long-term commitment to use. The best of our studies show that if people stop semaglutide they will regain about two thirds of the weight they lost over the next year. Those numbers will vary person to person, but the overall message is that this is an ongoing treatment.
Then there is the issue of cost. Currently few drug insurance plans cover weight loss medications. In Canada, we are waiting with bated breath as Ozempic is going to potentially become available in a generic version in the spring of 2026. We are expecting the cost of this medication to come down but don’t yet know how profound that decrease will be.
There are also side effects of semaglutide, mostly related to the way the medication slows the forward motion of the stomach and intestines. Approximately 20% of people experience nausea, vomiting, constipation and/or diarrhea, often with starting the medication or increasing the dose; side effects usually settling down over a short period of time.
As you’ve probably guessed, Nic, these are challenging side effects in our SCI population. Constipation can be a trigger for autonomic dysreflexia, and diarrhea is a completely unpleasant experience when living with an SCI.
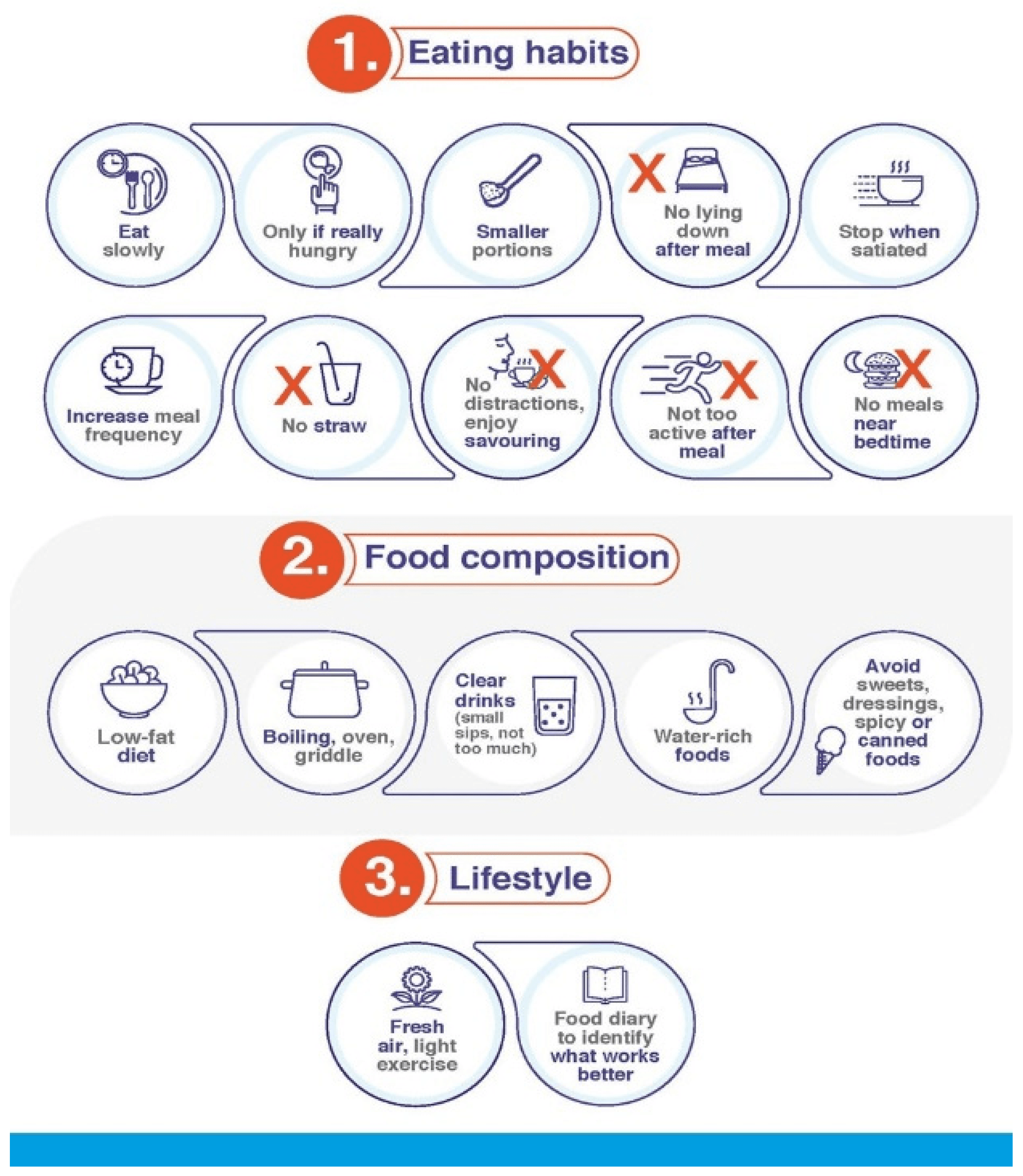
There are a couple of good principles to help limit the risk of gastrointestinal effects:
- Make your meals smaller and more frequent, which will decrease the risk of nausea.
- Avoid high fat food, as it tends to decrease forward motion of our stomach and intestines and lead to worsening nausea and constipation.
- Before you start the medication, it is useful to have your bowels in good working order with adequate fibre and lots of water.
- These medications often signal us to drink less. So, set a timer on your phone to remind you to drink water regularly, which is particularly useful to avoid constipation.
- Finally, if these medications are causing severe or persistent side effects, please speak to your doctor as decreasing the dose will often address
these issues.
The image below is one of several infographics created by an expert consensus group that provide easy to follow guidelines for managing gastrointestinal effects of the medication.
These new weight loss medications are a powerful tool for our health, but the best results happen together with good nutrition and physical activity. Good nutrition (especially adequate protein), and regular physical activity maintains our strength, muscle mass, and metabolism during weight loss which are key aspects of good health and independence.
So, if you’re struggling with unhealthy weight, is Ozempic an option? The answer is nuanced, but it may be worth asking your doctor if it is right for you.
This article was originally published in the Winter 2025 issue of The Spin. Read more stories from this issue, including:
- Mindfulness
- Adaptive skateboarding
- Menopause
And more!





