It turns out that one of the best medicines for chronic pain might not be a medicine at all. New research shows that exercise can help reduce SCI-related chronic pain.

A new scoping review published recently by BC researchers in the journal Spinal Cord suggests that physicians treating chronic pain for patients with SCI should consider prescribing physical activity and exercise, along with medications.
Over the years, there’s been some credible research that suggests exercise is a good way for some people to alleviate SCI-related chronic pain—both muscular pain and neuropathic pain. The scoping review, conducted at Dr. Kathleen Martin Ginis’ SCI Action Canada Lab at UBC Okanagan and led by graduate student Kendra Todd, is the first time all of this research has been summarized. These combined results leave little doubt that exercise and physical activity can result in improvements in both chronic pain and overall well-being.
The review, titled Physical activity interventions, chronic pain, and subjective well-being among persons with spinal cord injury: a systematic scoping review, began with an exhaustive literature search to identify all relevant and credible studies from around the globe that have attempted to measure the effects of “leisure time physical activity interventions” on both chronic pain and at least one measure of subjective wellbeing—for example, life satisfaction.
A total of 3,494 articles were screened. Of these, just 15 published articles, describing 12 different studies, met the review inclusion criteria. “Of these 15 articles, 12 concluded that exercise led to reductions in pain and improvements in well-being for people with SCI,” says Todd, a PhD student in UBC’s School of Health & Exercise Sciences. “Interestingly, the exercise that was prescribed within these articles varied and included multiple types of aerobic and resistance training. Perhaps the most critical finding of this scoping review was that not one single study reported that participants experienced increased pain and worsened well-being as a result of exercise. Also, an important take-home from these studies was that exercise can improve multiple types of pain, including neuropathic or musculoskeletal—but the frequency and intensity of exercise matters.”
Todd also adds that the review reveals the shortcomings of research done to date on the subject. For one, the mechanisms behind these improvements are poorly understood. “Chronic pain is a complex biopsychosocial phenomenon with biological contributors such as tissue damage, psychological contributors including a person’s level of coping skills, and social contributors like social relationships,” says Todd. “Any combination of these components can impact a person’s pain experience. One possible reason for exercise leading to improvements in chronic pain and well-being is that exercise can increase levels of serotonin, which is a mood stabilizing hormone and influences nervous system cell interaction. However, mechanistic causes of pain development vary between the different ‘types’ of pain—for example, neuropathic or musculoskeletal—and I would like to be cautious not to overgeneralize.”

Another problem made clear by the scoping review is that researchers working in this field have never been on same page when it comes to using the same types of exercises for testing.
“These inconsistencies prevent researchers from identifying the appropriate frequency, intensity, time or type of exercise required to lead to the largest improvements in chronic pain and wellbeing among persons with SCI. Future research should use consistent exercise protocols—particularly protocols that adhere to the SCI Exercise Guidelines— in order to accurately compare results across studies. Furthermore, future research should continue to test the effects of exercise on both chronic pain and well-being using evidence-based theories, in order to identify mechanisms responsible for these effects.”
Regardless, Todd says that the review concludes there is enough evidence to alter how physicians treat patients with SCI experiencing chronic pain.
“Currently in Canada, pharmaceuticals are the most commonly-prescribed treatment for neuropathic and musculoskeletal pain among persons with SCI,” she says. “One reason for this is that there is a lack of controlled research investigating alternative types of management options, which inhibits clinicians from prescribing anything other than medications. Based on the developing evidence, it appears that exercise could be incorporated into an individual’s pain management program because it may have positive impacts. At the very least, exercise should be considered by clinicians alongside currently prescribed pharmaceuticals such as gabapentin and baclofen. However, it’s important for people to monitor how new treatments, exercise included, impact their pain fluctuations, as any treatment is not a one-size fits all approach. As we know, everybody’s SCI is different and therefore one person’s experience with exercise as a treatment for pain may vary from others.”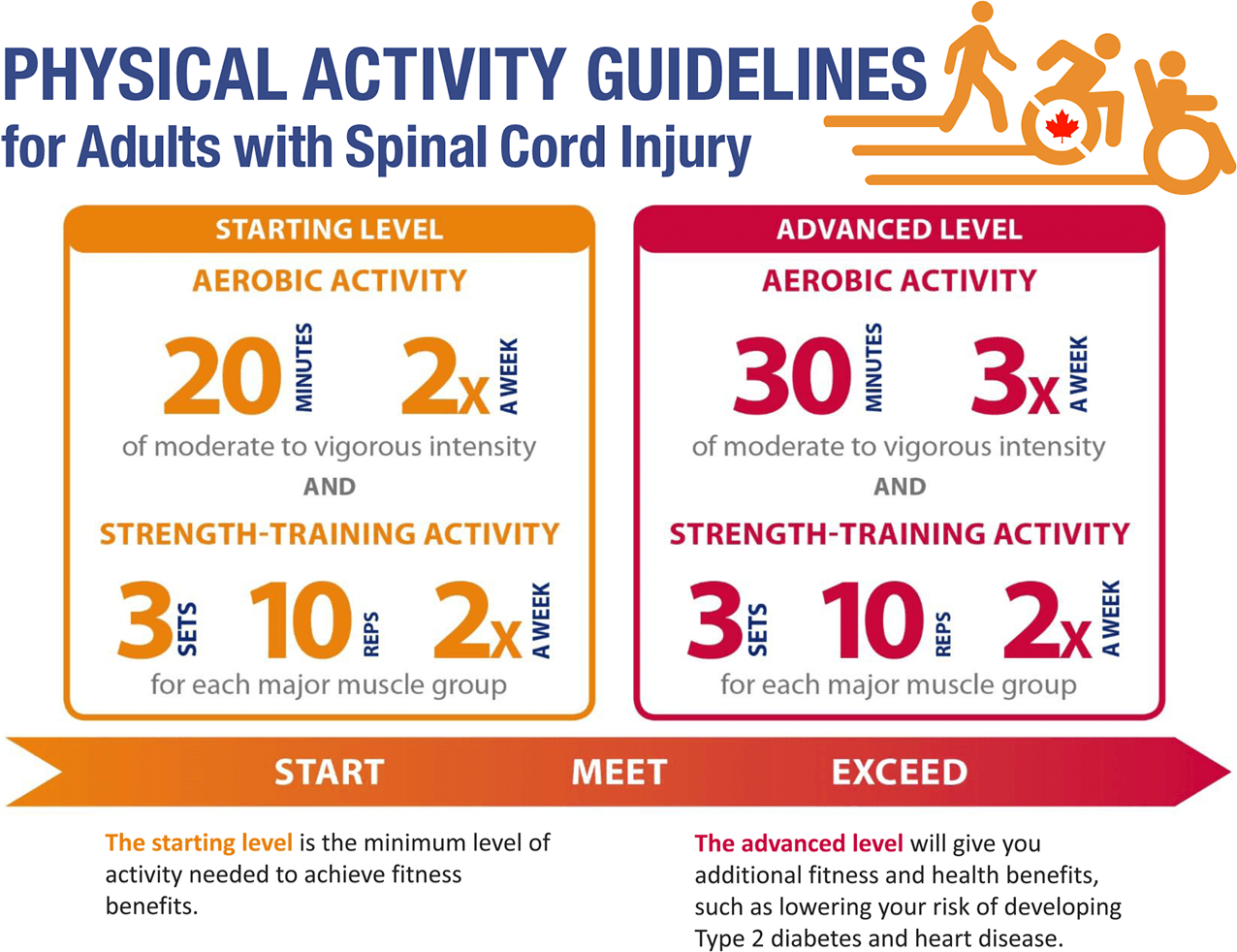
Given the evidence summarized in this review, and that exercise is generally accepted as safe, readers might consider making a decision to get on the exercise train without doctor’s orders. And remember that there’s a host of proven benefits of exercise above and beyond being an analgesic.
“In addition to pain relief, exercise participation may benefit a person’s health in other ways such as reducing the risk of cardiovascular disease, helping to control spasticity, decreasing the incidence of pressure sores, and stabilizing blood sugar and insulin levels,” concludes Todd.
If you’d like to learn more about your options for exercise and physical activity, a great place to start is to learn more about the Physical Activity Guidelines for Adults with SCI—see the infographic above, and visit sciguidelines.ubc.ca for more information and resources.
Looking for new ways to get active? Check out this invention from one of our members.
 This article originally appeared in the Winter 2020 issue of The Spin. Read more stories from this issue, including:
This article originally appeared in the Winter 2020 issue of The Spin. Read more stories from this issue, including:
- UTI & Pressure Injury Treatment
- Research on Exercise and Pain Management
- Winter Activities from our Community Partners
And more!



