It probably seems like we’re always fixated on bowel function here at The Spin. But the reality is that survey after survey of people with SCI make one thing clear: bowel routines are one of the biggest challenges you face, and you believe research in this area should be a high priority.
A couple of issues ago, we wrote about work being done in this area at Dr. Reggie Edgerton’s UCLA lab. Using their own proprietary technology, the SpineX SCONE transcutaneous stimulation device, Edgerton, along with Dr. Parag Gad and other colleagues, demonstrated that electrical impulses delivered by electrodes attached to target areas on the skin above the spinal cord were able to restore some sensation and induce contractions in the rectum. And in a case study of one person, a stimulation training regimen of one hour daily for one week resulted in a dramatic reduction of time needed to complete a bowel routine— from 75 minutes to 15 minutes.
This study, and others like it, have been performed with what’s known as an open loop stimulation system. It’s called open loop because the participants receive a pre-determined stimulation set determined by the researchers involved. The stimulation parameters—the timing, duration, strength and frequency of the pulses—are preset and remain constant throughout the treatment. It’s only after the results of the stimulation become apparent that the parameters can be adjusted for subsequent treatments.
These type of open-loop stimulation systems are relatively successful and well-established. But it may be that there is potential for better results using closed loop stimulation.
In a closed loop system, there are two components. Like an open loop system, closed loop systems have a stimulation device and electrodes that work together to deliver electrical pulses to the target nerve or muscle to trigger the desired outcome. But closed loop systems also have a component that senses, in real time, the effect of the stimulation and, after analyzing that feedback, automatically and dynamically adjusts the stimulation parameters as required to increase the effectiveness of the therapy—and to reduce troublesome side effects.
At Texas A&M University, Dr. Hangue Park and his colleagues are developing this type of closed loop stimulation system in an effort to replicate the natural rhythm of the digestive system and more normal bowel function after SCI.
“Although the effect of electrical stimulation on promoting effective colon movement has been previously investigated, no previous study has yet investigated the result of closed loop electrical stimulation on promoting colon movement,” says Park, an assistant professor in the Department of Electrical and Computer Engineering. “The motivation of this work is to offer people with SCI, as well as their caregivers, a higher quality of life.”
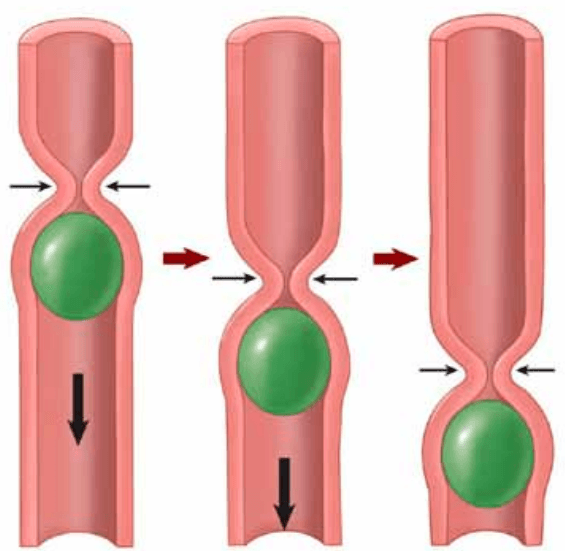
The underlying mechanism of a normal bowel movement is mass peristalsis—a natural, sequential and rhythmic constriction and relaxation of the muscles in the colon that propels stool to the rectum prior to voiding. It’s this process that is often compromised in people with SCI. The result is neurogenic bowel—constipation, incontinence, and the need for a routine that can take hours to complete.

Finding a way to safely trigger mass peristalsis in people with SCI would, in essence, cure neurogenic bowel. But how to do that? Despite promising results, the open loop stimulation using the SCONE device that we referred to above does not fully restore peristalsis. It appears to be more of a blunt instrument that stimulates the vagus and pelvic nerves to induce some peristaltic contractions in one part of colon.
The approach taken by Park and his colleagues at Texas A&M is to surgically-implant highly flexible electrodes at key points on the surface of the colon itself. These electrodes can trigger the adjacent rings of smooth muscles in the colon in a sequence that mimics peristalsis—and also seem to “reawaken” the nervous system’s central pattern generator for peristalsis. Meanwhile, sensors that are also implanted on the colon provide electrocolonogram monitoring to determine what’s happening with the colon in real time. Information from these sensors is assessed by a computer and used to immediately change the stimuli as required to continue peristalsis and propel stool to the rectum.
In 2019, Park and his colleagues published a paper for a conference titled A Real-time Electrocolonogram Monitoring and Electrical Stimulation System for Promoting Mass Peristalsis of the Colon. Here’s what the authors wrote in the paper’s conclusion: “We have developed a real-time electrocolonogram monitoring and stimulation system and evaluated its efficacy on promoting peristaltic movement with a mouse model. The results obtained during benchtop tests and animal experiments clearly showed that the presented system could simultaneously record electrocolonogram and induce colonic activity and initiate peristaltic movements of colon with electrical stimuli.”
Since that paper was presented, Park and his team have continued to refine their system and research methodology. Much of the work has focused on the timing of stimulation—determining when is the best time to initiate stimulation, which is a complex problem as the colon is still a mystery to researchers in many ways.
“With a series of experiments, we learned that e-stimulation should be carefully applied with a closed-loop optimization, based on the reading from the colon,” says Park, adding that timing of closed-loop stimulation is what gives it the potential to be a more effective therapy than the open loop stimulation.
“Timing of stimulation,” he asserts, “is a critical part for the efficacy of E-stim, and therefore closed-loop operation is inevitable.”
Another priority is to determine the optimal intensity of stimulation so that the effect is maximized, but without damaging the colon.
Recently, the Craig H. Neilsen Foundation announced financial support to Park and his colleagues so that they can move forward with their research.
“With the funding from Craig H. Neilsen Foundation, we are investigating how to optimize e-stimulation to recover the compromised colon motility after SCI, again using an animal model,” he says. “I would say this is a very important step to increase the efficacy of e-stimulation, which is necessary for the translation into a human clinical study. Investigation onto the potential side effects is also necessary to move forward for the clinical trials. I expect we need three to five years until the clinical trial.”
He cautions that there are other hurdles to clear before that human clinical trials will be possible.
“Miniaturization is a critical part for translation to human studies,” says Park. “And installing electrodes to the colon may require an abdominal operation, which carries its own risks.”
Meanwhile, researchers using non-surgical transcutaneous stimulators such as SpineX’s SCONE system are pushing forward with their own research to build on recent successes in bowel function stimulation, and approval for actual real world use by Health Canada and the FDA appears more and more likely in the foreseeable future. If this happens, and if people with SCI experience significant improvement in bowel function by using these devices that require no surgery, the closed-loop system being investigated by Park and his colleagues may have to offer a far more effective solution to be viable, given the potential complications of any surgicallyimplanted device.
Only time will tell if the closed loop system will offer people with SCI a normal bowel experience. At the very least, Park’s work is likely to contribute to our collective understanding of the digestive system after SCI—and what it takes to resolve one of its most troublesome secondary complications.
It should be noted that Park and his colleagues are currently working to publish new results of this ongoing project by year’s end. If the results are noteworthy, we’ll provide an update in a future issue of The Spin.
This article was originally published in the Fall 2022 issue of The Spin. Read more stories from this issue, including:
- Adaptive Clothing
- Canada’s First Chief Accessibility Officer
- SCI & Immunity
And more!
Read the full Fall 2022 Issue of The Spin online!




