The doctor is in! In our Spin Doctor series, we explore hot-button questions about SCI and disability from our peers throughout the province and share answers from healthcare professionals across disciplines.
Have a question of your own? Email thespin@sci-bc.ca to be featured!
Question:
“I find my spasticity is a lot better with exercise in general, but lately spasticity in my hips is causing me a lot more trouble than it used to. I stretch a lot and I try to spend time lying flat on my belly to stretch out, but I feel like I’m fighting a losing battle. The tightness makes me sore, especially when I wake up after lying flat all night, and can sometimes get in the way of things I want to do. I’m worried I won’t be able to use my standing frame or lie flat anymore if this keeps up. Is this the kind of thing that Botox could fix? Is there anything new on the spasticity horizon that I should know about? I really don’t like taking medications for spasticity—the side effects bother me a lot.” – Marci from Sydney, BC
Answer:

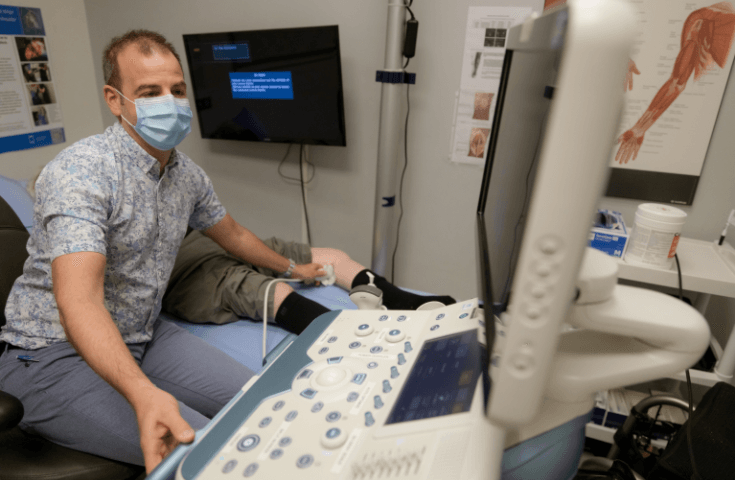
We turned to Dr. Paul Winston, a Victoria-based physiatrist who is Medical Director of Island Health Rehabilitation and Transition, President of the Canadian Association of Physical Medicine and Rehabilitation, co-founder of the Canadian Advances in Neuro-Orthopedics for Spasticity Congress, and co-founder of the Victoria Peripheral Nerves and Spasticity Clinic.
Spasticity and SCI
Spasticity affects up to 80 percent of people who live with SCI. Usually it remains quite steady. Any time there is an increase or change, it suggests that there may be some type of noxious stimulus in the body. So it’s important to first check for infections (such as a UTI), impacted bowels, pressure sores or skin breakdown,and even in-grown hairs and hemorrhoids. Broken bones, formation of new bone (heterotopic ossification), or a hip dislocation may also be the cause, and can be diagnosed with x-rays. Increased bladder pressure can also lead to an increase in spasticity. It’s important that your doctor or one of the many spinal cord injury physiatrists in the province rule out these possibilities.
Oral Medications for Spasticity and SCI
What happens when these investigations don’t turn up a cause? First, you raise a great point about committing to oral medications for a very long time. There are effective medications for spasticity, but they do have side effects of weakness and sedation, and some have effects on the liver. I usually avoid these if possible. If the spasticity is only in the hips, then taking a systemic drug for a focal problem is not the first choice, although some people do require medications and even need a Baclofen pump if spasticity is severe.
Injections
A thorough physical examination of the hips is required to see which muscles ,or muscle groups are the problem. Can you still put your legs flat on the bed, or press your pelvis onto the bed when on your tummy? Do your legs squeeze together, or do your knees bend up to the waist? These questions need to be answered. Once specific muscles are found to be the cause, botulinum toxin injections may be quite helpful. They serve to lengthen spastic muscles and stop their involuntary pull. Keep in mind that, if the pull is really strong, botulinum toxin can have limited benefit. There are many muscle groups we can try to target. Phenol, an alcohol, may be used to as well with specialized guidance.
It might take some time to work out an effective course of treatment. But there is something you can do in the interim—have the muscles stretched by a family member, friend or therapist if you can’t do it yourself.
Cryoneurotomy
At the Victoria Peripheral Nerve and Spasticity Clinic, we’re studying novel ways to treat spasticity by freezing nerves (cryoneurotomy) at -60 degrees Celsius, and performing small microsurgeries to target nerves and tendons. For certain muscle groups, we can temporarily paralyze muscles with nerve blocks to see which muscle is the most responsible. Orthopedic surgery may be required in severe cases.
Every case of spasticity is a unique pattern that requires a very thorough assessment. It may take several trials to find the optimal treatment. I would suggest you ask your family doctor to make a referral to a spasticity expert.
More Resources
Read our resources on spasticity
More about cryoneurotomy
Find out about intrathecal baclofen therapy
This Spin Doctor question was originally featured in The Spin 2020 Spring Edition



