
We are fortunate in BC to have some of the best health care professionals and community service providers dedicated to supporting people with SCI, but the reality is that not everyone can access them when they need them. Our health systems are under immense stress and key infrastructure is aging and in need of renewal. Decades of budget belt tightening have disproportionately put the squeeze on rehabilitation and recovery care and services, resulting in inequitable access to care and services and a loss of true expertise in SCI. It may not be fair to say the system is broken, but it is obvious that it is severely challenged and that many people with SCI and other conditions are suffering unnecessarily as a result.
Times of challenge, however, present times of opportunity. And there is now an incredible opportunity to reshape our system of rehabilitation and recovery. But how? This is the question two parallel, complementary, collaborative, community-centred initiatives set out to answer.
The BC Rehabilitation and Recovery Strategy and Advocacy Plan (the BC R&R Strategy) project is a collaboration between the Heart & Stroke Foundation, SCI BC, After Stroke BC / March of Dimes Canada, the BC Brain Injury Association and Brain Wellness Program, researchers, health professionals, and individuals with lived experience of SCI, stroke, and brain injury. Funded through a grant from the Vancouver Foundation and facilitated by the Emily Carr University Health Design Lab, the project examined post-hospital rehabilitation and recovery across SCI, stroke, and brain injury.
As a member of the BC R&R Strategy steering committee, SCI BC helped co-design a series of twelve online workshops with health care professionals and people with lived experience of SCI, stroke, and brain injury. Held in the spring of 2022, the workshops set out to understand the experience of people who both work and live with British Columbia’s current system of rehabilitation and recovery for these three diagnoses and to learn about their ideas to improve that system.
In all, 49 people participated in the workshops, including 7 SCI peers and 11 health professionals and researchers from across the province. The SCI Care Strategy is an SCI community-led initiative facilitated by the Rick Hansen Foundation that is engaging health authorities, practitioners, and researchers, and is closely informed by individuals with SCI. Whereas the BC R&R Strategy focused on post-hospital rehab and recovery, the BC SCI Care Strategy focused on all aspects of care for traumatic and non-traumatic SCI – from the time of injury onward. As an actively engaged partner in both initiatives, SCI BC has played a central role in coordinating communication between them.
Between the two initiatives, over 200 persons with lived experience, practitioners, researchers, and organizations shared their experiences within the system and insights on how to improve it. And while the two strategies used different approaches to gather this input, what was heard was so similar that it was possible for the two initiatives to develop a joint set of recommendations for advancing rehabilitation and SCI care in BC.
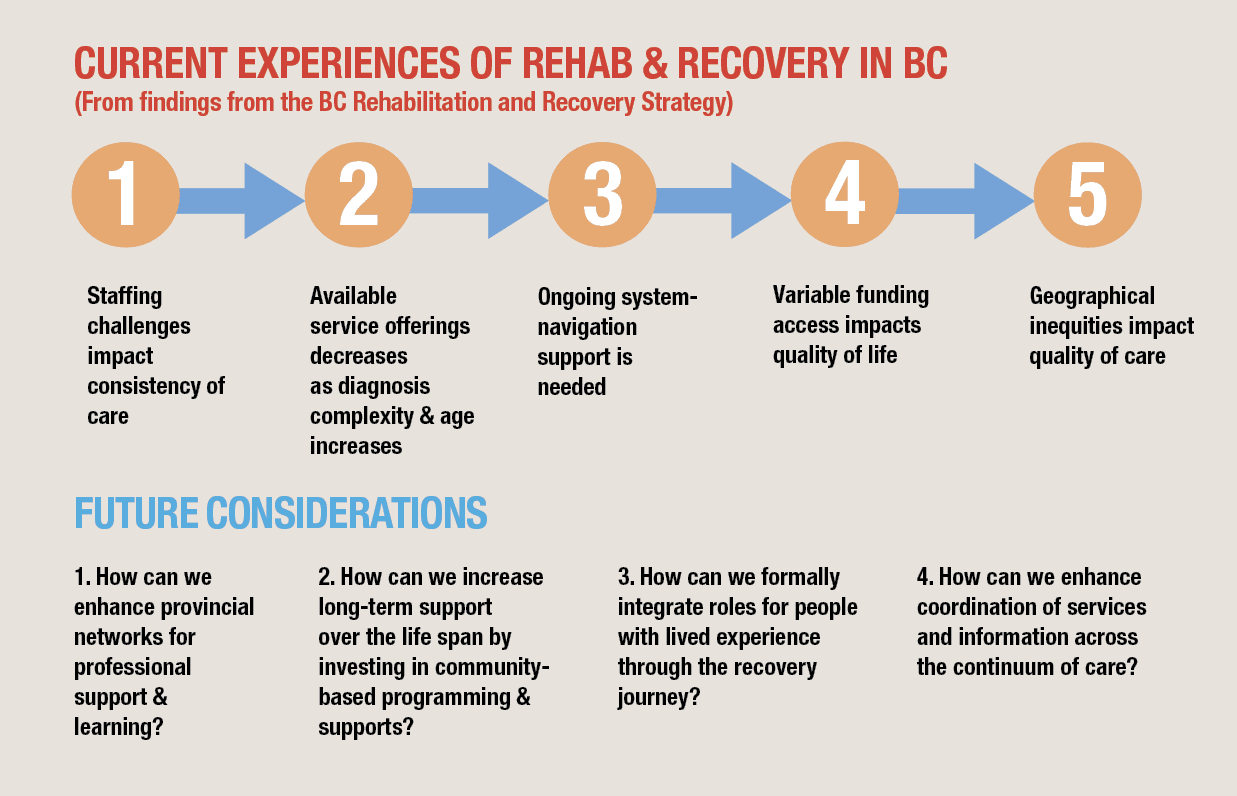
The joint recommendations will be made public soon, but in the meantime, we can provide you with a summary of what it will contain. Currently, the system faces two core structural challenges. One is the barriers to provincial coordination of health and community services, a challenge reinforced by the artificial boundaries created by the way our health authorities are set up. This lack of provincial coordination compromises transitions during different phases of one’s journey as a patient and community member. It also adds to the burden of navigating through different health systems and services. The other is a lack of capacity when it comes to appropriate health care infrastructure and rehab professionals with SCI expertise. This creates major hurdles and reinforces regional and social inequities to accessing care and services.
When it comes to imagining a new model of care in SCI, there first needs to be a recognition that SCI (and stroke and brain injury) is a lifelong condition that requires ongoing, specialized health and community services. A coordinated systemic approach to these services and information about and how to access them is required. For this to happen, rehabilitation must be viewed as a provincial priority, with more practitioners and providers, equipment and spaces, and research to better meet the needs of those impacted by these and other injuries. Having centralized SCI expertise and specialized centres is necessary, alongside regional capacity building and use of technology to sustain excellence and consistency in care across BC.
Along with these high-level recommendations, nine priorities the province should act on have been put forward. These priorities range from establishing a BC-wide agency responsible for a provincial rehab strategy and integrated care model to creating roles for peers in the system, to ensuring people with SCI, stroke, and brain injury have the financial supports, housing, and essential needs and services to maximize their health and quality of life.
9 PRIORITIES for improving BC’s system of rehabilitation and recovery for SCI, stroke, and brain injury.
- Create a BC-wide agency with responsibility for establishing a rehabilitation strategy and integrated care model.
- Operationalize a hub-and-spoke network of practitioners and facilities, through training and mentoring, mobilization of specialist multidisciplinary clinics, and greater use of technology to extend patient reach, notably in rural and remote locations.
- Expand acute care infrastructure to fulfil unmet and expected new demand, including facilities renewal and alignment of governance and funding at GF Strong as an anchor for broader system redesign.
- Establish a program of trained navigators, with roles for peers with lived experience, to support patients and their families in making the transitions from acute care to the community and to facilitate connections with health, community care, and social services and programs.
- Institute income support for those unable to work and not covered by WorkSafe or ICBC, in addition to non-means tested support to ensure access to essential care, equipment, and services.
- Increase funding for physiatrists and allied health professions, as well as home service workers, and align post-secondary training accordingly, to help assure timely access to experienced health practitioners.
- Formalize resourcing for the network of community groups operating in stroke, SCI, and brain injury, leveraging their autonomy and on-the-ground experience to enhance information and supports for people living with these and other chronic neurological diagnoses.
- Create more transportation options for short- and long-distance patient transfers to strengthen patient experience and the ability to attend work and access health care and other services.
- Consistent with the broader provincial housing agenda, develop more inclusive and accessible accommodation – from transitional housing post discharge to specialized long-term care to affordable homes – improving both patient lives and utilization of high-cost acute facilities.
We know the recommended changes cannot be made soon enough, but the reality is that there is much more work to do. The work done so far has set a general plan for the rehab and recovery system’s own rehab and recovery journey. The next phase of the journey will require the development of a detailed operational case for change and political will to support it. This will take time, but some changes can be made sooner and more easily than others. With so many of us working together, the push for change is a strong one. We’ll keep you posted on the progress we make.
This article originally appeared in the Summer 2023 issue of The Spin. Read more stories from this issue, including:
- Adaptive waterskiing
- Cannabis and chronic pain
- Information for newcomers with disabilities
And more!




